Getting the most out of MIPS can feel like a puzzle, especially when you’re aiming for the best possible payment adjustments. This guide breaks down how to approach MIPS reporting, understand the scoring, and make smart choices to help you achieve Maximum Reimbursement for MIPS. We’ll cover everything from who needs to report to how to pick the right measures, so you can focus on what matters most: your patients.
Understanding MIPS Eligibility and Exclusions
Before you can strategize for maximum reimbursement under the Merit-based Incentive Payment System (MIPS), you first need to figure out if you are even required to participate. It’s not a one-size-fits-all deal, and knowing where you stand is the first step. Think of it like checking the guest list before a party – you need to know if you’re invited!
Identifying MIPS-Eligible Clinicians
Generally, if you bill Medicare Part B for physician services, meet the low- volume- threshold, and aren’t part of an Advanced Alternative Payment Model (APM), you’re likely considered a MIPS-eligible clinician. This includes most doctors, physician assistants, nurse practitioners, and clinical nurse specialists. However, if you’ve opted out of Medicare entirely, MIPS doesn’t apply to you. It’s all about your relationship with Medicare Part B claims.
Navigating Low-Volume Thresholds
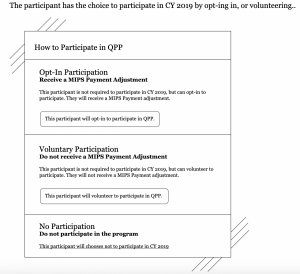
CMS sets specific thresholds to determine who is exempt. For a given performance year, you’re exempt if you bill less than $90,000 in Medicare Part B allowed charges, see fewer than 200 Part B patients, or furnish fewer than 200 covered Part B services. If you meet any one of these criteria, you fall below the low-volume threshold and are excluded from MIPS. It’s important to check these numbers annually, as they can change. You can use the CMS MIPS Lookup Tool to verify your status. In addition, if you meet one of the LVT criteria, you can also choose to “opt-in” to MIPS and attempt to achieve a positive payment adjustment.
Recognizing Exemptions and Special Statuses
Exemptions and special statuses for the Quality Payment Program (MIPS, MVPs and APP Programs) can be found beyond the low-volume threshold. Some of these include new Medicare enrollees, Advanced APM participants, and those practicing in Health Professional Shortage Areas. Understanding eligibility is crucial for effective MIPS strategy, avoiding missed opportunities or unnecessary burdens.
Here’s a quick rundown of common exemptions:
- New Medicare participants
- Qualifying participants in Advanced APMs
- Clinicians below the low-volume threshold
- Clinicians who have opted out of Medicare
Remember, even if you’re exempt, you can still choose to report MIPS data. If you choose to opt- in, it will indeed result in a payment adjustment, so carefully review and make the best business decision for your practice. Opting in when not required can provide valuable insights into your performance compared to national benchmarks and prepare you for when you may eventually become fully eligible.
Deconstructing the MIPS Composite Score
Your MIPS composite score is the big picture, the final number that tells Medicare how well you’re performing across all 4 categories within the program. Think of it like building a house – you need a solid foundation, good walls, a roof, and all the interior furnishing to make it complete. Each part matters, and how they’re weighted can shift a bit year to year, but the core components stay the same.
The Quality Performance Category
The Quality Performance Category showcases the quality of care, a major part of the score. It involves selecting measures that demonstrate the service’s quality, with one measure being outcome, patient safety, efficiency, or care coordination. This category builds on older reporting systems such as PQRS, and requires a full year of performance data.
The Cost Performance Category
Medicare uses claims data to track healthcare costs, tracking patient care expenses. To accurately link patients and services, claims must be coded correctly. This category is becoming a larger part of the overall score, emphasizing understanding of practice costs.
Promoting Interoperability Category
Promoting interoperability essentials involves using certified electronic health record (CEHRT) technology to improve patient care. Hardship exceptions may be available for small practices, older systems, poor internet, or challenging circumstances. Reporting on measures earns points, demonstrating connectivity and effective data sharing. Certain measures within the category are required and cannot be excluded. In addition, a CERHT ID from the EHR is required for submission of data to this category.
The Improvement Activities Category
The Improvement Activities Category is a category for practice improvement by completing various activities for at least 90 days. These activities are categorized as high, medium, or low impact. To get full credit, a combination of activities is required. Small practices, health professional shortage areas, and patient-centered medical homes may receive lower requirements.
Strategic Reporting for Maximum Reimbursement for MIPS
CMS is introducing MIPS Value Pathways (MVPs) to group measures by specialty, providing a comprehensive view of a practice’s value across quality, cost, and improvement activities. These measures, like QCDRs and virtual group reporting, can streamline MIPS reporting and potentially improve collective performance, especially for mental/behavioral health.

-
Leveraging Qualified Clinical Data Registries (QCDRs): Using Qualified Clinical Data Registries (QCDRs) simplifies MIPS data collection and submission, potentially boosting overall score. These registries, like Patient360, handle data collection and submission, and QCDR measures are directly approved by CMS, reducing back-and-forth processes.
-
The Advantages of Virtual Group Reporting: Virtual group reporting, available since 2018, allows solo practitioners or small practices to pool resources and report as a single entity, streamlining MIPS reporting and potentially improving collective performance, provided members meet low-volume thresholds.
-
Exploring MIPS Value Pathways (MVPs): CMS is introducing MIPS Value Pathways (MVPs) to group measures by specialty, providing a comprehensive view of a practice’s value across quality, cost, and improvement activities. The program is expected to become more prominent as CMS phases out the traditional MIPS program and eventually cover all specialties.
Achieving Exceptional Performance Status
Achieving exceptional performance status in MIPS signifies excellence within the Quality Payment Program (QPP). This status results in high payment adjustments, impacting financial health of the practice.
Understanding Exceptional Performance Bonuses
- CMS recognizes exceptional performance with a positive payment adjustment.
- The positive payment adjustment is an additional incentive for clinicians who exceed standard requirements.
- The adjustment amount can fluctuate based on overall program performance and the number of clinicians achieving this status given it’s a budget neutral program.
Strategies for Top-Tier Scoring
- Select high-value quality measures aligning with practice’s strengths and patient population.
- Optimize resource utilization and patient outcomes in the Cost category.
- Maximize use of certified EHR technology and advanced functionalities in Promoting Interoperability.
- Choose improvement activities that significantly impact patient care and practice operations.
The Impact of Performance Thresholds
- CMS sets annual performance thresholds defining exceptional performance.
- Consistently high scores across all categories are the most reliable way to surpass these targets and qualify for bonuses.
Leveraging Support for Maximum Reimbursement for MIPS

Navigating the complexities of the Merit-based Incentive Payment System (MIPS) can feel like a solo expedition, but you don’t have to chart this course alone. Fortunately, there are several avenues of support designed to help you maximize your reimbursement and streamline your reporting process. Think of these resources as your seasoned guides, offering insights and practical assistance.
Accessing CMS Technical Assistance Programs
The Centers for Medicare & Medicaid Services (CMS) provides direct technical assistance to help clinicians understand and comply with MIPS requirements. These programs can offer clarity on measure selection, reporting methods, and overall program strategy. Don’t underestimate the value of direct guidance from the source. They can help you avoid common pitfalls and identify opportunities for improvement.
Utilizing Quality Innovation Network Resources
Quality Innovation Networks-Quality Improvement Organizations (QIN-QIOs) are regional partners that offer support to clinicians, particularly small and rural practices. They often provide educational materials, training sessions, and personalized assistance tailored to MIPS reporting. Connecting with your local QIN-QIO can be a smart move to get practical advice.
Engaging with Alternative Payment Model Learning Systems
Alternative Payment Models (APMs) often have learning systems that provide resources and support for their structure and alignment with MIPS or MIPS Value Pathways. Understanding these connections can optimize performance and maximize reimbursement. Proactive engagement with these systems is crucial for meeting MIPS requirements and excelling within the program, aiming for better outcomes for practice and patients.
Want to get the most money back for MIPS? Patient360 can help you understand how to use support systems to your advantage. Learn how to make MIPS work for you and get the best results. Visit our website today to find out more!
Putting It All Together for Better MIPS Results
MIPS is a program that helps medical professionals improve their reimbursement results by focusing on areas that matter most to their practice and using the right tools. Staying informed about the program’s changes is crucial, as it is constantly evolving. Adjusting reporting, exploring QCDRs or virtual groups, and staying updated on CMS updates can help make the system work for you. Seeking help is also recommended.