You’ve probably heard about MIPS, the program that adjusts Medicare payments based on how you perform. It’s been around for a bit, but things are changing. If you’re a clinician, you need to know about this new direction. It’s not just about reporting anymore; it’s about adapting to a system that’s evolving. Let’s break down what you need to know about the Clinicians New Direction of MIPS.
Key Takeaways
- The Merit-Based Incentive Payment System (MIPS) is shifting away from its traditional structure.
- MIPS Value Pathways (MVPs) are becoming a bigger part of the program, offering a more focused approach.
- Expect changes in how quality and cost are measured, with a greater emphasis on interoperability.
- Practice management needs to adapt to these changes, especially for smaller or rural practices.
- The long-term goal is to move towards payment models that better reflect value in patient care.
Understanding the Evolution of MIPS
The Shift from Traditional MIPS
The Merit-based Incentive Payment System (MIPS) has significantly transformed the way healthcare providers are paid for their services. MIPS consolidates older programs like the Physician Quality Reporting System and Value-Based Modifier, aiming to simplify payment structures. The system focuses on performance metrics, technology usage, and service cost, tying payments to quality and cost performance.
Key Changes Impacting Clinicians
MIPS has undergone significant changes over the years, with a focus on patient-centered outcomes and data quality. Clinicians must stay updated with new measures, weights, and focus on interoperability and digital tools for effective patient care management.
The Rationale Behind Program Adjustments
The government is adjusting Medicare payments to align with value, aiming for better care at lower costs. They are aiming to shift the healthcare system towards a model where providers are rewarded for maintaining health rather than just treating patients. The changes aim to simplify reporting while ensuring high-quality care and reducing healthcare spending.
Navigating MIPS Value Pathways (MVPs)

What constitutes an MVP?
MIPS Value Pathways (MVPs) are specialized tracks that group measures and activities relevant to a specific medical field or patient condition. They aim to simplify reporting, make performance measurement more meaningful for practice, and make it feel more connected to day-to-day work, rather than a vast list of potential measures in traditional MIPS reporting.
The Expanding MVP Framework
CMS is expanding its MVP framework, proposing new pathways for various specialties in 2026. These include Diagnostic Radiology and Interventional Radiology, along with existing ones for Cardiology and Mental Health. This expansion signifies that these pathways are becoming a central part of the MIPS program.
MVP Participation: An Evolving Landscape
The MIPS Value Pathways (MVP) program is becoming increasingly popular as it offers a streamlined way to meet MIPS requirements. While it is still optional, it represents a significant shift in how clinician performance is measured and rewarded. It is essential to monitor the development of these pathways to align with practice goals.
Adapting to New Quality and Cost Strategies
As the MIPS program evolves, you’ll need to adjust how you approach quality and cost performance. It’s not just about ticking boxes anymore; it’s about genuinely improving patient care while managing expenses. This means looking closely at how your practice measures up and where you can make meaningful changes.
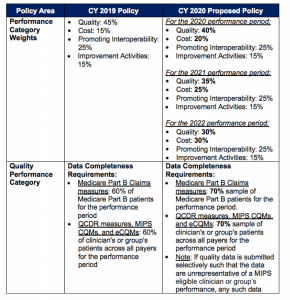
Revisiting Performance Categories
The core performance categories within MIPS are being refined. You’ll see shifts in how quality measures are selected and scored, with a continued push towards measures that reflect real-world outcomes. Expect a more streamlined measure inventory, with some measures being removed and others updated to better align with current healthcare priorities. This is your cue to re-evaluate which measures are most relevant to your patient population and practice goals. It’s also a good time to explore new quality measures that might better showcase your practice’s strengths.
The Role of Interoperability and Digital Measures
Interoperability and the use of digital measures are becoming increasingly important. Think about how your electronic health record (EHR) system can support data sharing and automated reporting. The focus is shifting towards measures that can be captured digitally, reducing the manual burden of reporting. This move is designed to make data collection more efficient and the data itself more accurate. Embracing these digital tools can also provide you with more timely insights into your performance.
Aligning with Future Payment Models
MIPS efforts should prepare for future healthcare payment shifts, with value-based care models becoming more common. It’s crucial to align quality improvement initiatives with potential future payment structures. Understanding Quality Payment Program policy is key to aligning data collection and reporting strategies, ensuring performance reflects actual care quality.
Implications for Practice Management
Impact on Small, Rural, and Safety-Net Practices
- MIPS changes may impact small, rural, and safety-net practices.
- These practices may have limited resources for data collection and reporting.
- New MIPS requirements should align with practice capacity and patient demographics.
- Measures focusing on digital patient engagement may be challenging for practices with limited access or older patient populations.
- The program should not widen existing care or access gaps.
Addressing Reporting Burdens
MIPS reporting requirements can be overwhelming, but integrating electronic health records and third-party reporting solutions can streamline the process. Training staff on new data entry protocols and reallocating responsibilities can help make reporting an integrated part of quality improvement efforts. Automated data capture could be a game-changer.
Strategies for Value-Based Care Readiness
Getting ready for value-based care means more than just meeting MIPS requirements; it’s about shifting your practice’s mindset. This involves focusing on patient outcomes, care coordination, and cost-effectiveness. Consider these steps:
- Analyze your current performance: Where do you stand on key quality metrics? Identify areas where you excel and areas needing improvement.
- Invest in technology: Ensure your EHR system supports data extraction for quality reporting and patient engagement. Look into tools that can help with population health management.
- Team training: Educate your staff on the principles of value-based care and their role in achieving quality goals. This includes everyone from front desk staff to clinicians.
- Patient engagement: Develop strategies to involve patients more actively in their care, such as through patient portals, outcome tracking, and personalized care plans. This aligns with measures like Beneficiary Engagement (BE).
The transition to value-based care is a marathon, not a sprint. It requires a sustained commitment to improving patient outcomes and managing resources efficiently. Focus on building a culture of continuous quality improvement within your practice.
As you adapt to these changes, remember that understanding the nuances of measures like Population Management (PM) can significantly impact your practice’s performance and reimbursement. Staying informed about how quality of care is assessed is key.
The Future Trajectory of Clinician Reimbursement

As you look ahead, it’s clear that how you’re paid for your services is changing. The focus is shifting from just doing more to doing better. This means your practice needs to be ready for different ways Medicare might pay you down the line. It’s not just about MIPS anymore; it’s about being set up for value-based care in general.
-
The Long-Term Vision for MIPS: The Centers for Medicare & Medicaid Services (CMS) proposes changes to the Medicare Physician Fee Schedule for 2026, keeping the MIPS performance threshold at 75 points, aiming to reward quality and efficiency of care, rather than volume.
-
Advocacy for Payment System Reform: AMA advocates for Medicare payment system reform, including tying payments to MEI and fixing budget-neutrality rules. Strengthening Medicare for Patients and Providers Act (H.R. 2474) aims to create a stable, predictable payment system, benefiting practices of all sizes.
-
Ensuring Equitable Performance Measurement: The current MIPS system, intended to reward quality, has been criticized for being too burdensome and not always relevant to daily patient care. Advocacy efforts aim to reduce reporting burdens and ensure quality measurement accurately reflects patient outcomes, supporting high-quality care delivery.
Thinking about how doctors get paid in the future? It’s changing fast! We’re keeping up with all the new rules and how they affect your practice. Want to know more about what’s coming next for doctor payments? Visit our website to get the latest updates and tips.
Looking Ahead: Navigating the Evolving MIPS Landscape
The MIPS landscape is evolving, shifting from strictly adhering to rules to embracing MIPS Value Pathways. Traditional MIPS remains in place, but the direction is clear. It’s crucial to monitor these pathways and their impact on practice, reporting, and performance. Understanding these changes is essential to avoid being caught off guard and stay prepared for future quality reporting challenges.