You’ve probably heard about the 2026 Medicare Physician Fee Schedule Proposed Rule and are wondering what it means for you. It’s packed with proposed updates on MIPS, six new MVPs, easier ACO reporting, a new program model, and a chance to shape the final rule via multiple RFIs. We’ll walk you through the highlights and show you how a QCDR like Patient360 can help. Let’s get to it.
Breaking Down the CY 2026 CMS-1832-P Proposed Rule
The Centers for Medicare & Medicaid Services (CMS) has dropped its Medicare Physician Fee Schedule proposed rule for 2026, and, as usual, it’s a hefty one. This proposed rule, officially known as CMS-1832-P, outlines significant changes including those to the Physician Fee Schedule (PFS), the Quality Payment Program (QPP), and Medicare Shared Savings Program (MSSP). It’s important to understand how these changes could affect your practice, your reporting, and ultimately, your revenue. The Medicare PFS proposed rule is over 1,800 pages, so let’s break down some key areas.
Key Takeaways
- The MIPS performance threshold is proposed to remain at 75 points through 2028.
- The transition from Traditional MIPS to MIPS Value Pathways (MVPs) continues with additions (6 new MVPs) and changes to the inventory of MVPs.
- Other MVP-related proposals include changes to the registration process whereby multispecialty groups split into subgroups through self-attestation while allowing small multispecialty groups the option to maintain small group status.
- The Quality and Improvement Activities categories are proposed to have several additions, removals, and changes.
- While only a change to a single Cost measure is proposed, future Cost category planning offers flexibility for providers and QCDRs for future new Cost measures.
- Modest Promoting Interoperability changes include modifications to the EHR SAFER Guide measure, suppression of the Electronic Case Registry requirement, and a new optional bonus measure.
- If you’re in an ACO, there are only minor proposed changes, leaving you more time to focus on improving quality measure reporting and adjusting to the APP program in general since Web Interface retired in 2024.
- CMS is also proposing a new program called the Ambulatory Specialty Model (ASM) that focuses on chronic conditions of Heart Failure and Low Back Pain to start with performance year 2027.
- CMS is asking for your feedback in RFIs on a number of topics such as FHIR rollout, the PDMP measure, and adding well-being and nutrition measures.
Think of it this way:
- The proposed rule is like a blueprint for how physicians and other providers will be paid.
- It’s influenced by laws and policies already in place.
- It’s subject to change based on feedback from people like you.
Keeping up with these changes can feel like a chore, but it’s important. Your payments, your reporting requirements, and even the way you deliver care can be affected. A QCDR partner like Patient360 can keep you organized, help you report on time, and hit those pay-for-performance goals.
What’s Proposed in MIPS for the 2026 Performance Year
You should be aware that the MIPS 2026 performance year is likely to bring several changes. CMS is aiming for program stability and simplification while advancing priorities like reducing burden, preventative care, and outcomes-focused assessment. The proposed regulations contain important updates that will affect your reporting and performance.
MIPS Performance Threshold Holds Steady at 75 Points
Good News! For providers participating in the Merit-based Incentive Payment System (MIPS), the performance threshold is proposed to remain at 75 points for 2026, 2027, and 2028 performance years. This means you’ll need to continue to achieve at least this score to avoid a negative payment adjustment. Maintaining this threshold requires a continued focus on high-quality care and efficient resource utilization. It’s a good idea to monitor your ongoing 2025 results in Patient360 throughout the performance period. Lessons learned indicate that monitoring your data early and often is best practice; at least once a month is encouraged. In addition, you should also review your 2024 Feedback Report/Scores in QPP by logging in as a security official for your TIN by the fall of 2025, which is likely when final scores will be released. Being informed about your past performance is a great way to make informed decisions and set attainable goals moving forward.
Quality & Improvement Activity Measure Inventory Changes
CMS continues to advance priorities to reduce process measures in favor of outcome measures, remove measures with topped out benchmarks, and focus on meaningfulness and driving improvements in care. Overall, CMS proposes to add 5 new, remove 10, and make substantive changes to 32 MIPS Clinical Quality Measures. Selecting measures that best represent your clinical area and ensuring accurate data collection and reporting are key to optimizing your score in this category.
For the Improvement Activities category, CMS proposes to add 3, modify 7, and remove 8 activities while adding a new subcategory called Advancing Health and Wellness and removing the Achieving Health Equity category.
Changes to the Cost Category
CMS is proposing to score cost measures and provide 2 years of informational-only feedback on new measures starting with the 2026 performance year. This feedback on new cost measures is designed to help you understand your performance in this area and give you insights into your cost efficiency before these measures fully impact your MIPS score and payment adjustments.
Another shift from last year is that CMS is NOT proposing to add or remove any cost measures for 2026. They do propose changes to a single cost measure: Total Per Capita Cost (TPCC). The overall inventory of 35 cost measures comprises 33 that are episode-based measures and 2 population-based measures.
Promoting Interoperability Changes: TEFCA Bonus & Measure Suppression Policy
CMS is proposing Promoting Interoperability changes that include modifying the Security Risk Analysis measure and the High Priority Practices Safety Assurance Factors for Electronic Health Record (EHR) Resilience (SAFER) Guide measure. Additionally, they propose to add the Public Health Reporting Using Trusted Exchange Framework and Common Agreement (TEFCA) as an optional bonus measure. Regular opportunities from CMS rewarding participants bonus points for proactive engagement are crucial for practice optimization and participation, and avoiding negative payment adjustments. Incentivizing TEFCA participation is another option to encourage proactive planning to meet requirements and maximize Promoting Interoperability category scores. To achieve the bonus, clinicians would need to attest that they’re in active engagement with a public health agency to transfer health information using TEFCA.
Another layer of flexibility CMS is proposing for the Promoting Interoperability category in 2026 is the ability to suppress measures, as they do at present with other categories in the QPP for various reasons. When a measure is suppressed from a category, this usually results in a denominator reduction and doesn’t impact the overall score negatively and proposing this suppression option will align more with the quality category scoring methodology. One of the PI measures CMS is proposing to suppress is the Electronic Case Reporting measure for the current 2025 performance year.
Six New MVPs and Flexibility for Multispecialty Small Practices
The CY 2026 proposed rule introduces six new MVPs, aiming to expand specialty options. These new pathways are designed to better reflect the diverse range of specialties and care settings. This expansion intends to offer clinicians more relevant and manageable participation options and will be for the following specialties: Diagnostic Radiology, Interventional Radiology, Neuropsychology, Pathology, Podiatry, Vascular Surgery. Opportunities to provide feedback and comments on these newly proposed MVPs can be made via the public commenting opportunity provided by CMS here.
It was previously finalized that as of the 2026 performance year, “multispecialty group” will no longer be a registration option for MVPs; they must instead register and report as subgroup(s) or individual. In this proposed rule, CMS proposes to allow multispecialty groups to self-attest to the relevant area(s) of specialty focus when they subdivide into and register as subgroups. Furthermore, multispecialty groups that are small practices (i.e., 15 or fewer clinicians) would retain the option to register as a group and will not be required to register as subgroups.
Minor Changes Proposed for 2026 MSSP ACO Reporting

For 2026, there have been minor changes proposed, with the goal to continue to streamline MSSP APP reporting. Here are a few of the main changes proposed:
- Definition revision of eligible beneficiaries for Medicare CQMs
- Removal of Health Equity Adjustment applied to ACOs quality score
- Removal of Quality ID: 487 Screening for Social Drivers of Health
- CAHPS survey changes for 2027 (Expanding administration protocol to web – mail – phone)
- Expansion of EUC policies for ACOs to include those impacted by cyber attacks
Regarding the APP Plus Quality Measure Set for 2026, if the proposal is finalized, MSSP ACOs will NOT need to report Quality Measure 487, but they WILL need to report Quality Measure 113: Colorectal Cancer Screening, which was finalized in the 2025 Final Rule. Quality measures 112 & 113 for the APP Plus Quality Measures Set will continue to maintain flat benchmarking for 2026, while the other Quality Measures within the set 001, 134, & 236 will likely have historical benchmarks applied since they will have been in use for 2 years. Although proposed changes to the MSSP ACO reporting are fairly minor for 2026, it’s still important to use time and resources wisely to focus on documenting well for all measures within the set, along with harnessing integration and data flow early, often, and consistently.
NEW Program Model!!! Ambulatory Specialty Model (ASM)
CMS has proposed a new test model scheduled to launch in 2027. This model is intended to promote prevention, upstream management, and timely, targeted care of low back pain and heart failure to help patients stay in good health and keep their cost of care low. While there are many aspects of the model that mirror the MIPS/MVP program such as data completeness, timing of payment adjustments, benchmarking, and the same 4 categories (Quality, PI, IAs, & Cost), there are a few key differences:
- CMS is proposing the following clinician specialty types will be required to report at the individual level and if eligible, will NOT report MIPS/MVPs. Note: there will be no group reporting:
- Heart Failure Cohort: Clinicians who have been assigned a cardiology speciality code on their Medicare Part B claims
- Low Back Pain Cohort: Clinicians who have an anesthesiology, interventional pain management, neurosurgery, orthopedic surgery, pain management, or physical medicine and rehabilitation speciality
- Heart failure and low-back pain episode-based cost measures will be part of determining eligibility along with the plurality of Medicare Part B claims
- Payment Adjustments will follow the same 2 year cadence as MIPS, but CMS is proposing to retain a percentage of the payment adjustment rather than distributing all funds as payment adjustments to participating clinicians
- ALL measures within the Quality Measures model will be required. Clinicians cannot pick and choose. These are the proposed sets:
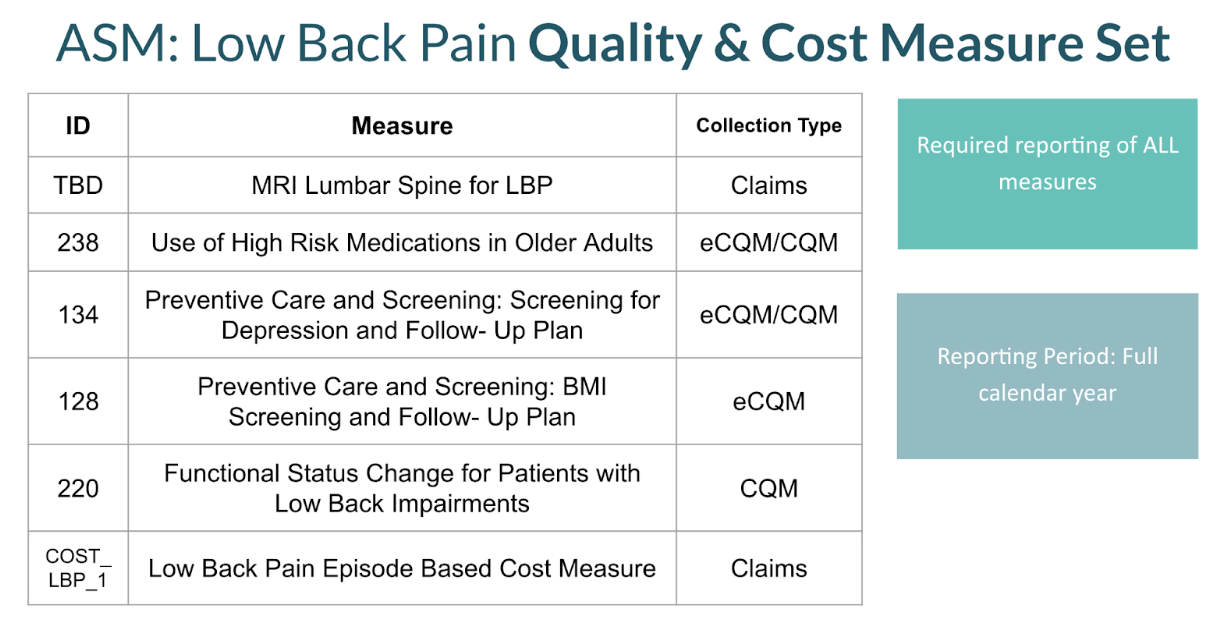
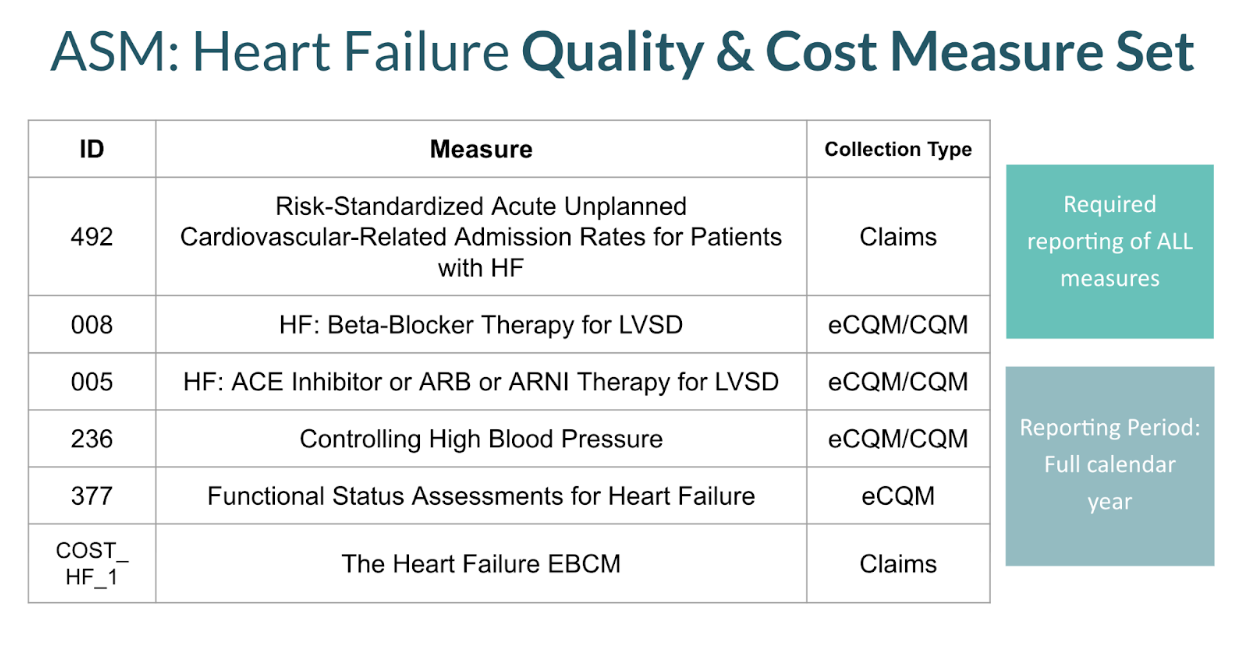
The new model being proposed is detailed for nearly 300 pages within the proposed rule; so it’s a significant new proposal. CMS has requested ample feedback and comments. Therefore, if the model impacts your specialty and you are a current MIPS/MVP participant, it’s imperative you provide your feedback: Comment on the 2026 Proposed Rule.
CMS Wants Your Feedback! RFIs to Monitor

CMS isn’t just dictating changes; they’re actively seeking your input on several key areas. This is your chance to shape the future of healthcare regulations and ensure they work for you, your patients, and your organization. Pay close attention to these Requests for Information (RFIs) – your voice matters!
FHIR, PDMP, MVP Core Elements, and Well-being & Nutrition Measures
CMS is exploring some interesting new directions, and they want your thoughts. Here’s a quick rundown of just a few of the RFIs contained within the 2026 Proposed Rule:
- FHIR Interoperability: They’re looking at ways to accelerate the adoption of Fast Healthcare Interoperability Resources (FHIR) to improve data exchange. How can FHIR be used to streamline workflows and improve care coordination? They have had multiple RFIs in the past couple of years on FHIR, so it’s evident this is a top priority.
- Prescription Drug Monitoring Programs (PDMP): CMS is soliciting feedback on shifting this PI measure from an attestation measure to a performance based measure (which would include denominator and numerator elements) as well as expanding the types of drugs that would apply to the measure.
- MVP Core Elements: CMS is soliciting feedback on which measures should and shouldn’t be included in the Core Elements and the impact those selections may have on clinician decision making to adopt the MVP.
- Well Being & Nutrition Measures: CMS is soliciting feedback on tools and measures that can be utilized to improve overall health and well being proactively and preventatively.
This Proposed Rule contains more RFIs than other previously released Proposed Rules. If you are overwhelmed by providing feedback on all of them, perhaps select one or two that are most relevant to you, your practice, and your patient population. Don’t miss out on providing your valuable feedback because these RFIs are indeed the appropriate forum to do so and we know from experience that they are carefully assessed by CMS.
Consider these points when formulating your feedback on the proposed rule.
Have Your Say:
How to Submit Feedback on CMS-1832-P
CMS wants to hear from you! These proposals aren’t set in stone, and your input can directly influence the final regulations. The Centers for Medicare and Medicaid Services (CMS) is actively soliciting feedback on various aspects of this proposed rule, and it’s important to make your voice heard.
Submitting your comments is a key way to shape the future of Medicare policy.
Here’s what you need to know to participate:
- Review the Medicare Physician Fee Schedule Proposed Rule: While reading the entire 1800 pages of the full text of the CMS-1832-P proposed rule can take more time than you have – or want – to give, CMS provides fact sheets and press releases (on cms.gov) that can help you hone in on the select issues that are most relevant to your practice, specialty, or organization. From there, you can navigate to those specific sections of the full text to understand the full detail. Understanding the details is essential for providing informed feedback. You can find the proposed rule in the Federal Register 2026 Medicare Physician Fee Schedule
- Prepare Your Comments: Organize your thoughts and write clear, concise comments that address specific aspects of the proposed rule. Be sure to provide supporting data or evidence whenever possible. Explain how the proposed changes would impact your patients, your practice, or the healthcare system as a whole. CMS recommends all comments include a structured format that details the page and comment you are responding to, the potential issue you have identified, the direct impact of the issue, and your proposed alternate solution.
- Submit Your Comments: You can submit your comments electronically through the Federal eRulemaking Portal (Regulations.gov). Follow the instructions on the website to submit your comments by the deadline. Make sure to reference the CMS-1832-P proposed rule in your submission.
The deadline for submitting comments on Medicare policy is September 12, 2025. Participate to shape the future, ensuring the final rule reflects patient and provider needs.
Partnering for Success: How Patient360 Simplifies the 2026 CMS Transition
Patient360 is a QCDR partner that simplifies reporting and compliance with CMS requirements. They help healthcare providers understand new rules, implement necessary changes, and ensure success in the 2026 performance year. Patient360 offers expert guidance, simplified reporting, and real-time data to help healthcare providers stay ahead of the curve. They provide updates on key CMS regulatory changes (proposed rules), simplify data submission, and identify opportunities to improve MIPS scores and reimbursement. Patient360 is committed to providing tools and support to help practices thrive in the evolving healthcare landscape, reducing administrative burdens and allowing them to focus on patient care.



