Since no one has time and likely very little inclination to read 808 pages of government documentation on an already burdensome MIPS program, Patient360 has you covered! The following few pages give you a down and dirty summary of what you need to know.
While some positive aspects exist for 2020 (a.k.a., “Year 4”) QPP, there are also significant changes for 2021 and beyond. Some might even seem overwhelming. However, remember Patient360 is here to get you through any challenges and the open comment period allows you to speak your mind. In fact, we encourage you to let CMS know what you think. At the end of the blog we tell you exactly how to make that happen.
Let’s start with what has not changed for 2020, Year 4:
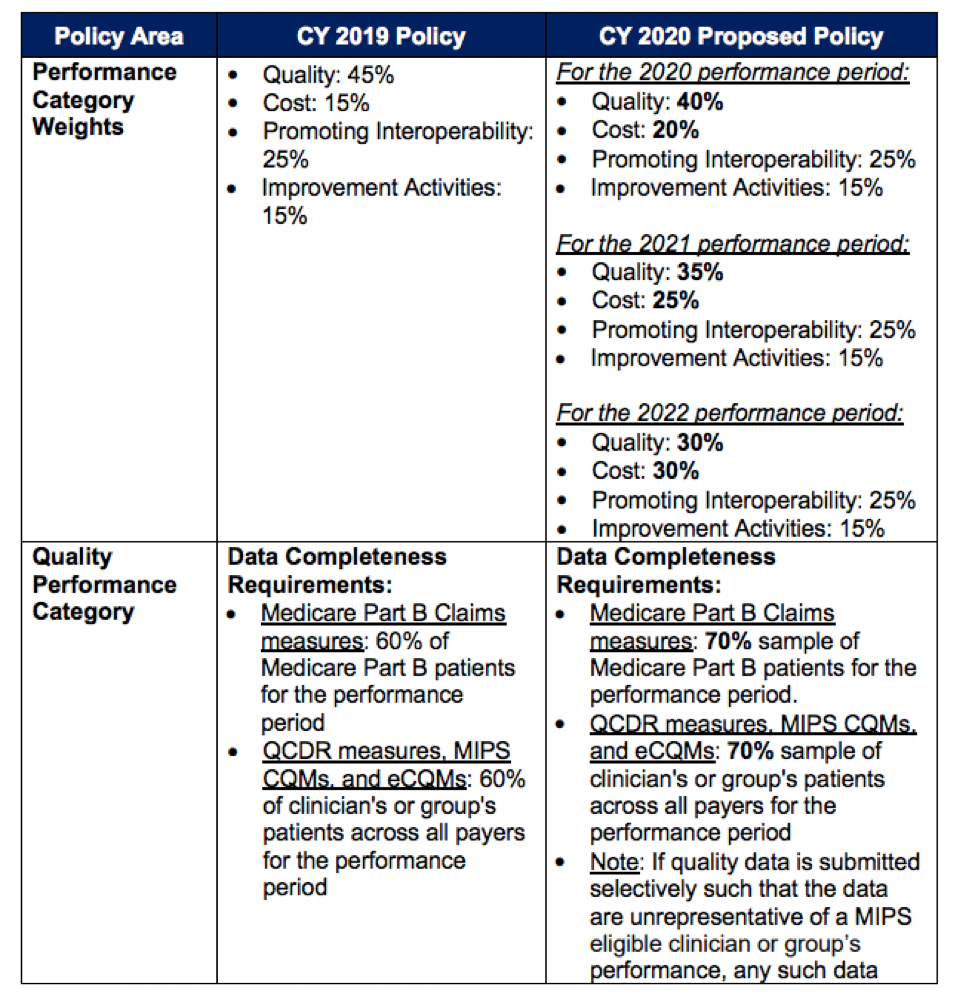
Next, some minor proposed changes for 2020, Year 4:
Basically, category “weight” is changing slightly by putting more emphasis on Cost. This 5% increase was expected based on previous indication from CMS. The value of Data Completeness has increased to 70% for each quality measure vs. 60%. Again, this was expected and we will most likely see it continue to rise until it reaches 100% of patients being reported. The CMS folks want TIN/EINs (tax identification numbers, a.k.a., employer identification number or EIN) to stop cherry picking and instead focus on improving quality of care across their entire patient population.
2021 and Beyond:
Now that we know 2020 isn’t really going to change significantly, focusing on 2021 and beyond is essential to prepare for what you can expect AND be empowered as part of the solution. Patient360 has ingested and publicly commented on multiple Proposed Rules throughout the history of the program. We can say with confidence that although the changes proposed are significant, CMS does truly want stakeholder and clinician feedback! CMS understands many of the policies outlined in the Proposed Rule are not fully baked. They want providers to collaborate and speak up about measures neither reducing burden nor really improving quality of care.
So out of 808 pages, what are the most significant changes for Patient360 clients to focus on? For sure it’s the new MVPs; i.e., MIPS Value Pathways.
Here is a picture of what that could look like:
Essentially these new “pathways” combine pre-selected, specialty focused measures from all of the current categories. Simply put, complete one (1) MVP containing pre-selected measures from each category and you’re done. The benefit is there will be far fewer measures and activities needed to meet the one (1) required MVP vs. many measures with a host of combinations. In other words, at present, reporting is across multiple categories (e.g., IA, Quality, etc.) with numerous elements in each category. A secondary benefit is pre-formatted/selected measures. Basically, under MVPs, just report the MVP and requirements are met. Sounds great, right? Mostly, yes. However, grey areas exist and stakeholder input is necessary:
- Since CMS plans to choose exactly which measures belong in the MVP, what happens if you submit an MVP but some of the measures in that MVP are not applicable to your TIN/EIN? Remember the legacy PQRS program’s Measures Groups? MVPs are somewhat similar. Again, measure selection is predetermined so a bit easier but options will be more limited. MVPs demand a TIN/EIN report ALL required measures within the MVP, or reporting won’t be successful.
- Who decides which specialty should be reporting which MVP? CMS is intimating MVPs be assigned to specific specialties. Right now, providers and groups have the option to select which measures and reported categories allow them to perform and “score” in the most optimal fashion. Limiting measures and mandating certain MVPs based on specialty creates potential trouble if your work is not “traditional” or more complex when compared to specialty group peers. Read the rules and offer comment or be assigned which measures you will be mandated to submit. Performance be damned!
For full details on the new MVP policies, begin on page 249 here.
Through previous public comments and stakeholder input, CMS leadership believes there has been too much choice with MIPS. Too much choice, they surmise, has led to confusion and a burdensome program.
What do you think? Patient360 encourages your TIN/EIN to provide feedback on the MVP policy being proposed. If you have time and feel passionate regarding the Proposed Rule, until September 27th make a comment at this URL.
No time to deal with government documentation and the commenting process? No worries! Send a simple email to Amanda with your feedback and comments. We will aggregate all comments and submit them on behalf of Patient360 TIN/EINs. The changes being proposed are significant, so it’s important for CMS to know what you truly think. Even if you only have time to write 2 or 3 bullets, it’s worth it! And, we’d love to hear from you.