The 2022 Quality Payment Program Final Rule
CMS released the 2022 Quality Payment Program (QPP) Final Rule. We will walk you through the details below, but you can also find additional resources on the 2022 Quality Payment Program website which provide useful visuals describing changes to the program compared to prior years.
Summary
In short, there were no surprises with the final 2022 QPP changes and the new requirements are fairly manageable. There are a few minor changes in terms of point allocation, bonus points, and category scoring percentages, but not much else has substantially changed for 2022 MIPS reporting with notable exceptions including a number of updates for APM Performance Pathway (APP) reporting and the future MIPS Value Pathway (MVP) program which now has 7 new MVPs approved. You can read more about these 7 approved MVPs here.
- The minimum performance threshold for 2022 will be 75 points; (i.e.75 points total across all MIPS categories is the minimum score to avoid penalty/negative payment adjustment.) This is a 15 point increase from 2021’s 60 points which means elevated performance is necessary to avoid negative payment adjustment, especially in a budget neutral program.
- 2021 was supposed to be the last year that CMS afforded exceptional bonuses. However, they did extend it through to 2022, although you will need to get at least 89 points total to be considered in the exceptional bonus territory. CMS describes this as follows:
We note that the 2022 performance year/2024 payment year is the final year for an additional performance threshold/additional MIPS adjustment for exceptional performance.
- The Quality performance category is worth 30 points, down slightly from 2021’s 40-point ceiling.
- The Cost performance category is up to 30 points from 2021’s 20 point maximum.
- The Promoting Interoperability (PI) category and Improvement Activities remain similar to 2021, at 25 and 15 points, respectively.
The Good News
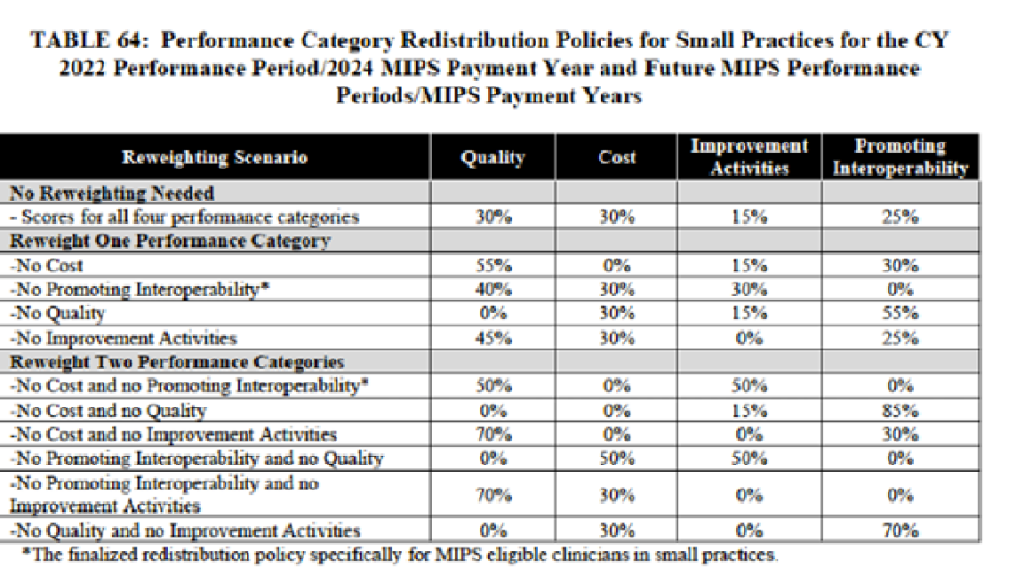
Small practices (under 15 clinicians according to the CMS eligibility criteria checker tool no longer have the burden of completing a PI hardship application for this category! If you are a small practice and choose not to submit any data for the PI category, it will automatically reweight to the Quality category. Below is a quick chart for small practices to see how various categories, including PI, will be reweighted:
The Bad News
Bye-bye to bonus points for additional outcome and high priority measures. Also, there is no longer an end-to-end electronic reporting bonus. Unfortunately it no longer matters how you report, even if it’s end-to-end, there are no additional bonus points for that method of reporting. While Patient360 formally rejected this removal of bonus points during the Public Commenting Period, CMS responded by letting all stakeholders know that they were federally mandated to remove these types of bonus points in time for the 2022 performance period.
The minimum threshold for data completeness while unchanged from 2021 continues to receive attention. As part of the 2022 Final Rule, clinicians must continue to submit greater than 70% of their patient encounters for each measure. Despite constant chatter bemoaning the perpetual elevated requirement, expect the rise to continue as CMS works to mitigate patient and measure “cherry picking.” Likely in 2023 this minimum threshold will move to 80%. CMS is essentially compelling providers to report as much data as possible for each quality measure vs. only the “best” data. CMS is focused on improving overall quality of care vs. demonstrating elevated performance on only a subset of patients. CMS recognizes that operational and technical situations may arise during the reporting period, and as such provide a mechanism to not have to report 100% of the numerator responses. .
Codifying Registry Obligations - Data Validation Audits:
Data validation audit requirements have not changed in 2022. The official codifying of registry obligation is to conduct randomized audits throughout the reporting year vs. just prior to the end of the reporting season/performance period. Registries are charged with eliminating erroneous data before it reaches CMS. “Detect and correct” is the standing compliance mantra! Conducting the data validation prior to data submission will lead to data being more reliable and promote compliance with the requirement of data being true, accurate, and complete. “In the CY 2017 Quality Payment Program final rule, we described this auditing using the term randomized audit.” These audits are a validation process that protect Patient360 clients and keep Patient360 in good standing with CMS. If you are interested in learning more, refer to this blog post which describes the importance of the auditing process, how it is used to achieve data integrity, and auditing best practices.
Originally presented as part of the 2020 Final Rule, the MIPS Value Pathways (MVP) program continues to receive COVID-related delays. MVPs will be officially launched in 2023 and require providers to report on a smaller set of measures. Theoretically, by limiting the volume of measures, CMS will be able to effect change more broadly. We believe these changes aren’t going to be made in a vacuum. CMS always seeks stakeholder feedback/comment on programs and is currently hosting multiple MVP Development Kick-Off Webinars. All stakeholders are encouraged to attend. Also, please know that the sunsetting of Web Interface collection and submission for ACOs has also been delayed until 2025.
If it seems tedious perusing dozens of appendices at the end of the Final Rule to learn which measures were retired or changed for 2022, here is a very quick snapshot. Remember, any questions, comments, concerns, or topics you’d like Patient360 to address, please let us know!
Measures with substantial changes:
87 CQM measures have changed – 1, 5, 7, 8, 9, 50, 65, 66,93, 102, 110, 111, 112, 113, 117, 119, 134, 143, 176, 177, 178, 180, 182, 217, 219, 226, 236, 238, 239, 240 , 254, 265, 281, 290, 291, 293, 305, 309, 310, 317, 318, 326, 335, 336, 340, 350, 351, 358, 366, 370, 374, 375, 376, 377, 378, 379, 383, 391, 395, 396, 397, 400, 409, 413, 416, 418, 425, 430, 438, 448, 450, 459, 460, 461, 462, 463, 469, 470, 471, 473, 476, 478 (As described in the 2022 Final Rule starting with page 2248)
13 CQM measures have been removed – 21, 23, 44, 67, 70, 154, 195, 225, 337, 342, 429, 434, 444. (As described in the 2022 Final Rule starting with page 2233)

